Rehab Articles
A new study by researchers at the University of Toronto shows that individuals who have schizophrenia also have a much higher risk of suicide, and that is not all that the study showed. Schizophrenic individuals who were victims of childhood physical abuse were 5 times more likely to attempt suicide as those who were not. For the population without schizophrenia the suicide rate is 2.8%, with schizophrenia the rate of suicide is a staggering 39.2% according to the results of this newest study. Lead study author Dr. Esme Fuller-Thomson reported “Even after taking into account most of the known risk factors for suicide attempts, those with schizophrenia had six times the odds of having attempted suicide in comparison to those without schizophrenia. Clearly those with schizophrenia are an extremely vulnerable population. Knowledge of the added risk of suicide attempts associated with childhood abuse and substance abuse could help clinicians improve targeting and outreach to this population.”
The researchers who explored the link between schizophrenia, physical childhood abuse, and an increase in suicide risks used a representative sample of more than 21,000 Canadians who responded to the 2012 Canadian Community Health Survey-Mental Health. 101 respondents reported having schizophrenia. Study co-author Bailey Hollister explained “When we focused only on the 101 individuals with schizophrenia, we found that women and those with a history of drug or alcohol abuse and/or major depressive disorder were much more likely to have attempted suicide.” The study researchers also found that traumatic experiences during childhood tended to strongly influence suicidal ideation in individuals.
Rehab Articles

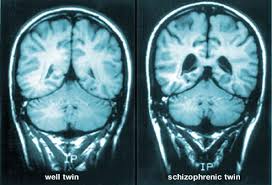
Antipsychotic drugs are commonly prescribed for those who have been diagnosed with schizophrenia, but recent research shows that these drugs can cause brain structure changes when they are used for a long term period. University of Brescia in Italy psychiatry professor and Spedali Civili Hospital psychiatric unit director Dr. Antonio Vita discussed the new research and stated “The role played by antipsychotic treatment on the pathophysiologic trajectory of brain abnormalities in schizophrenia is currently a matter of lively debate.” The study showed that more gray matter in the brain was lost when patients were placed on first generation antipsychotic drugs than what was lost when second generation drugs in this category were used. First generation drugs work differently in the body than second generation drugs in this class do, and that is a possible reason for the difference in gray matter volume and loss.
Dr. Vita treats patients with schizophrenia, and he has seen the imaging results which show the brain structure changes when antipsychotic drugs are used on a long term basis. Vita explained the new research by saying “Although this is a clinically meaningful result, many issues remain to be clarified. For instance, we still do not know whether the effects on the brain of antipsychotics vary as a function of age and stage of illness, or whether they may occur only when a certain threshold of exposure — daily dose or cumulative dose — is reached.. Clarification of these issues will have crucial importance in the clinical management of schizophrenia and will allow a better understanding of the mechanisms underlying the progression of structural brain abnormalities in the disease.” Have you or someone you know ever used these drugs?
Rehab Articles
When it comes to schizophrenia early intervention is very important. This step can help improve the quality of life for the patient, reduce the need for extensive and costly hospitalization due to this mental disorder, and improve the treatment outcome. With all of these benefits there is a shortage of early intervention programs and efforts that can make a difference. As soon as someone with schizophrenia starts to show signs that the mental disorder is worsening intervention should occur to prevent the symptoms from becoming worse. As this disorder progresses the individual may lose touch with reality, and it is common for hallucinations and delusions to occur when the disease worsens. These symptoms may put the patient at risk of harming themselves or others, leading to the need for hospitalization.
Early intervention when the first symptoms of schizophrenia start to show can make the difference between a hospital stay that could last for weeks or even months and the ability to stay out of the hospital and lead a better and more productive life. According to National Alliance on Mental Illness medical director and psychiatrist Ken Duckworth “All we ever saw in the ‘80s was the equivalent of stage 4 schizophrenia. It would be as if you were an oncologist, and all you saw were people with metastatic breast cancer.” Until now the focus has been on treating patients after symptoms worsen, but hopefully this will change and more public funding and support will be provided for early intervention programs as well. Do you know someone with schizophrenia who needs help?
Rehab Articles

A new study by King’s College London researchers shows that individuals with schizophrenia who have negative symptoms also tend to typically fair worse and have a worse outcome than those with this mental disorder who do not have negative symptoms. The patients who exhibited negative symptoms of schizophrenia had a much higher risk of admission to the hospital for this illness, the admission time was longer, and these patients were also more likely to be readmitted to the hospital after they have been discharged. Some of the negative symptoms that may be experienced include less speech and activity, poor motivation, and even failing to make eye contact with others. Positive symptoms include delusions and hallucinations, and these are usually the first symptoms targeted for treatment.
The study by the researchers is the biggest ever to look at and evaluate the link between clinical outcomes and negative symptoms for people with schizophrenia. The study involved sample cases from a pool of 7,500 individuals with schizophrenia. Department of Psychosis Studies researcher Dr. Rashmi Patel explained “Hospital admissions are the main drivers of cost in the care of patients with schizophrenia — yet they have traditionally been linked to the severity of positive psychotic symptoms. Our data indicate that negative symptoms are an equally important factor, and suggest that a greater emphasis on assessing and treating these features of schizophrenia may have significant health economic benefits. However, as our findings are drawn from observational data, interventional clinical studies are required to determine whether an effective treatment for negative symptoms would lead to better clinical outcomes.”
Rehab Articles
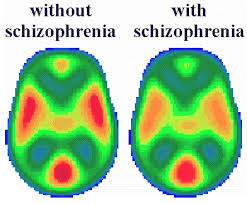
Brain imaging holds the key to why healthy siblings of schizophrenia patients avoid this disorder. The researchers n the latest study have found important differences in brain development during adolescence between those with schizophrenia and siblings who are healthy and do not have this mental disorder. The study showed that the healthy siblings experienced brain abnormalities similar to their schizophrenic siblings, but in the brain of the healthy sibling the brain development normalized and caught up with the development of normal teens without any indication of schizophrenia. Researchers hope that the latest brain imaging results and findings could open up new treatment possibilities. A partnership between researchers from the National Institute of Mental Health in Washington, D.C and the University of Melbourne in Australia made the study possible.
The brain imaging schizophrenia study used magnetic resonance imaging (MRI) technology to map out the brain development and patterns of 109 individuals who developed childhood-onset schizophrenia between the age of 12 and 24 years old. According to University of Melbourne electrical engineer and lead researcher Dr. Andrew Zalesky “We’ve looked at the development of brain networks over the adolescent period, from childhood to early adulthood. Abnormalities detected early in the unaffected children normalize by age 16. So why are these brothers and sisters able to overcome the risk? Looking for these biological factors that protect a person from developing schizophrenia opens up a new direction in the search for treatments.” According to Melbourne Neuropsychiatry Centre at the University of Melbourne Dr. Christos Pantelis, a co-author of the recent research study, “New generation medications can help young patients manage their symptoms, but can have significant side effects. Our work has the potential to open up avenues towards earlier intervention with fewer side-effects that improve a child’s resilience to becoming ill. This is an interesting new direction, as it suggests the search for targeted psychiatric treatments for schizophrenia and psychosis requires following young people over time.”